UK health crisis: Sick children left to suffer as wait for care soars
Hundreds of thousands of British children are waiting for surgery with new figures showing the backlog has spiralled by almost 50 per cent in two years as National Health Service (NHS) leaders and doctors warn that adult care is being prioritized over children’s.
The NHS data reveals that in December 2022, at least 364,000 children were waiting for their turn for treatment, whereas, another 200,000 were in dire need of therapy.
“Lengthy waits are unacceptable for any patient, but for children and young people, waits can be catastrophic, as many treatments need to be given by a specific age or developmental stage. It is not the same as for adults. If you miss the right window to treat a child, or wait too long, the consequences can be irrevocable,” Mike McKean, vice-president of policy at the Royal College of Pediatrics and Child Health told The Independent.
McKean also said that the intensive care capacity was being “pushed to the limits.”
Ever since April 2021, the child surgery backlog figures have skyrocketed to a new high, and have risen up by 48 percent, observing a whopping 36 percent increase in the figures.
An analysis of the figures shows that almost 3,000 children were waiting more than 18 months in November, while more than 15,000 were waiting for more than a year.
Many surgeries are also being postponed or cancelled just because of the staff, bed shortages at the NHS.
A six year old kid, Rosie, whose name has been changed, was referred for brain surgery in November as she is at risk of having a stroke.
Rosie’s surgery was cancelled at the last minute last month just because of shortages in staff, as there were not enough pediatric intensive care nurses, her mother told The Independent.
“The surgeons, anesthetists, operating department staff, porters, recovery staff and countless others are all assembled, but they haven’t got enough specialist pediatric intensive care nurses to safely cover the intensive care unit.,” she said.
“They explain that this regional intensive care unit is busy, and some children can’t be moved because they’re still too ill. The surgical teams have each been making the case for which of the poorly or high-risk children should have tonight’s intensive care bed. It will not be our daughter.”
Last week, the NHS England said pediatric services were experiencing “significant pressures in emergency departments and pediatric intensive care units” alongside long-standing challenges such as “insufficient” bed availability.
“On the ground, it feels like it has gotten worse, not better, because there has been no specific funding for recovery to cover the disproportionate increase in complexity,” said Dr Michael Absoud, clinical academic at the Department of Women and Children’s Health at Kings College London.
Doctors and the NHS leaders warn that just because the data does not include written or telephone referrals, it becomes difficult to project the true scale actual official data, that is imagined to be of a much bigger number than the provided one.
A senior NHS source believes that the waiting lists had grown by 70 percent in some specialties between 2021 and 2023.
The Royal College of Pediatrics and Child Health expressed fears that children’s services would not feature in the government’s forthcoming major long-term plan for the NHS; the college has also urged the government to launch a strategy plan to manage children’s health.
With Britain gripped with the horrors of the cost-of-living crisis, its effects have clearly manifested onto the healthcare industry of Britain.
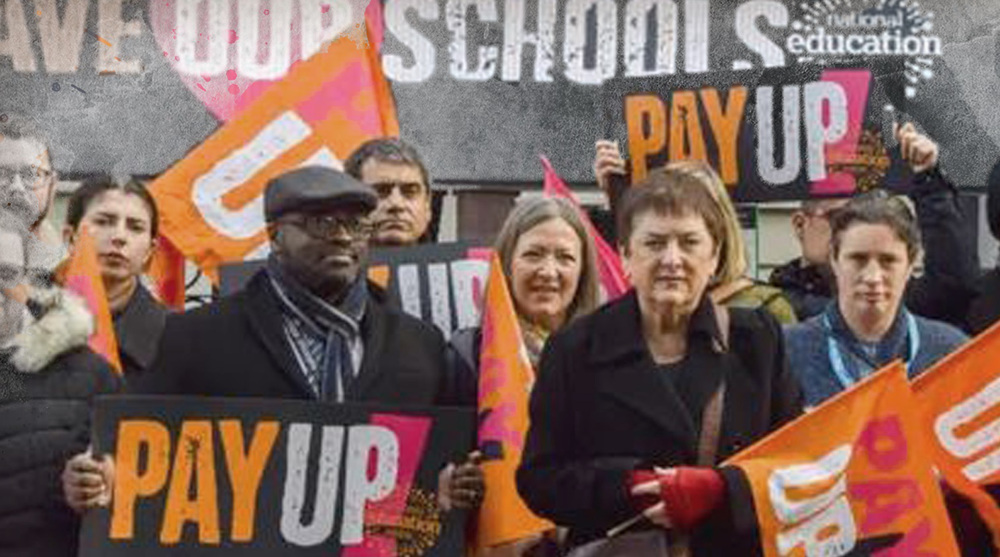
Since last year, ever since inflation was soaring at a record high in the UK, protests have continued ever since over pay.
The latest NHS nursing protest on Thursday, which was considered the largest such action in NHS history, saw tens of thousands of healthcare workers walking the streets demanding better pay, and had caused enormous disruptions to health services.
The Royal College of Nursing (RCN) had signaled that the strike would affect more than 120 NHS trusts across the country, far more than previous stoppages
US fighter aircraft shot down ‘in friendly fire’ amid aggression on Yemen
Yemeni FM: Israel’s sponsors accountable for ongoing aggression on Sana’a
Eight Palestinians killed as Israel attacks Gaza school, hospitals
VIDEO | Rome, Milan host new protests in solidarity with Palestinians
Dec. 21: ‘Axis of Resistance’ operations against Israeli occupation
Spain jurists demand ties with Israel ties be cut
VIDEO | Press TV's news headlines
VIDEO | Iran honors top Science Olympiad medalists


















 This makes it easy to access the Press TV website
This makes it easy to access the Press TV website